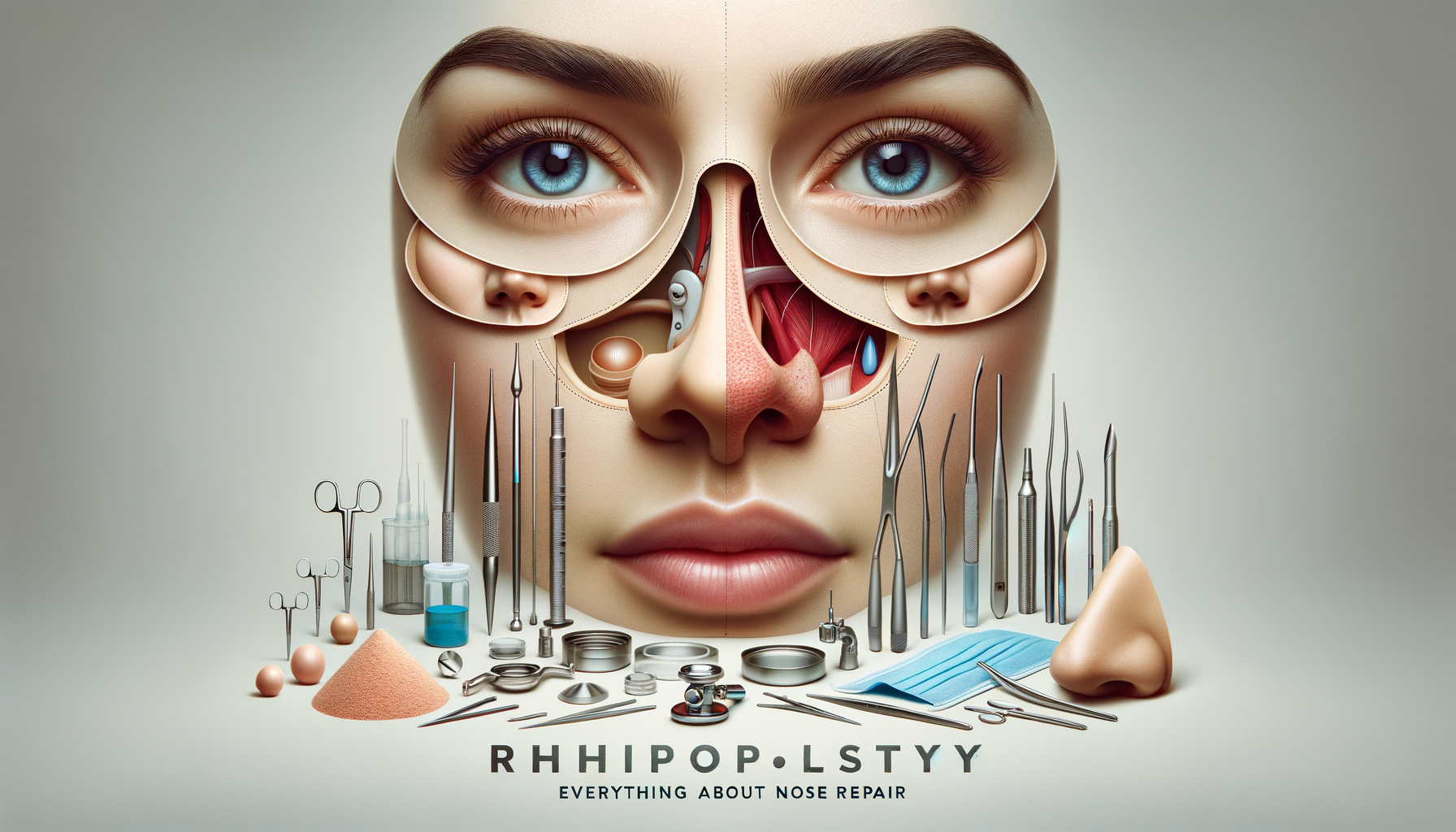
Understanding Reconstructive Rhinoplasty
Reconstructive rhinoplasty is a specialized surgical procedure aimed at restoring the nose’s function and appearance following trauma, congenital defects, or previous surgeries. Unlike cosmetic rhinoplasty, which primarily focuses on aesthetic enhancement, reconstructive rhinoplasty addresses both form and function. The importance of this procedure cannot be overstated, as the nose plays a crucial role in breathing and overall facial harmony.
Reconstructive rhinoplasty can involve several techniques, such as cartilage grafting, osteotomies, and septoplasty, to correct structural deformities. Surgeons often employ a tailored approach, considering the patient’s unique anatomy and needs, ensuring that the results are both functional and aesthetically pleasing.
The procedure may be necessary for individuals who have suffered nasal trauma, such as fractures or lacerations, or those with congenital anomalies like cleft palate. Additionally, patients who have undergone previous unsuccessful nasal surgeries may seek reconstructive rhinoplasty to correct any resulting issues.
- Restores nasal function
- Improves breathing
- Enhances facial symmetry
- Corrects congenital or trauma-induced deformities
Preoperative Considerations and Planning
Before undergoing reconstructive rhinoplasty, a thorough evaluation is essential. Surgeons conduct detailed assessments, including medical history reviews, physical examinations, and imaging studies, to understand the extent of the nasal deformity. This comprehensive approach ensures that the surgical plan is tailored to the patient’s specific needs.
Patients are encouraged to discuss their expectations and concerns with their surgeon. This open dialogue helps in setting realistic goals and understanding the potential outcomes and limitations of the surgery. Surgeons often use computer imaging to provide a visual representation of the expected results, aiding in the decision-making process.
Preoperative planning also involves considering the patient’s overall health and any potential risk factors that could affect the surgery’s success. Conditions such as hypertension, diabetes, or smoking can influence healing and should be managed appropriately before the procedure.
- Comprehensive evaluation and imaging
- Discussion of expectations and goals
- Management of health conditions
- Customized surgical planning
The Surgical Procedure
Reconstructive rhinoplasty is typically performed under general anesthesia, ensuring patient comfort and safety. The surgical approach can be either open or closed, depending on the complexity of the case and the specific corrections needed. In an open rhinoplasty, an incision is made across the columella, allowing the surgeon greater visibility and access to the nasal structures.
During the procedure, the surgeon may use cartilage grafts, often harvested from the patient’s septum, ear, or rib, to rebuild and support the nasal framework. Osteotomies may be performed to realign the nasal bones, and septoplasty might be necessary to correct a deviated septum, improving airflow through the nasal passages.
The duration of the surgery depends on the extent of the reconstruction required, typically ranging from two to four hours. Surgeons meticulously work to ensure that the final result is not only functional but also harmonious with the patient’s facial features.
- Performed under general anesthesia
- Open or closed surgical approach
- Use of cartilage grafts
- Osteotomies and septoplasty as needed
Postoperative Care and Recovery
After reconstructive rhinoplasty, patients can expect some swelling, bruising, and discomfort, which are normal parts of the healing process. Surgeons provide detailed postoperative instructions to aid recovery and minimize complications. These instructions typically include guidelines on wound care, activity restrictions, and medications to manage pain and prevent infection.
It is crucial for patients to attend follow-up appointments to monitor healing and address any concerns. The initial swelling may subside within a few weeks, but the final results of the surgery can take up to a year to fully manifest as the tissues settle and the nasal structure stabilizes.
Patients are advised to avoid strenuous activities, wearing glasses, and direct sun exposure during the initial recovery period. Adhering to these recommendations helps to ensure a smooth recovery and the best possible outcome.
- Swelling and bruising are common
- Detailed postoperative care instructions
- Importance of follow-up appointments
- Activity restrictions for optimal healing
Potential Risks and Complications
As with any surgical procedure, reconstructive rhinoplasty carries potential risks and complications. These may include infection, bleeding, scarring, or an adverse reaction to anesthesia. Additionally, there is a possibility of asymmetry or dissatisfaction with the aesthetic outcome, which may necessitate revision surgery.
To minimize these risks, choosing a qualified and experienced surgeon is paramount. Board-certified surgeons with extensive experience in reconstructive procedures are better equipped to handle complex cases and achieve satisfactory results. Patients should thoroughly research their surgeon’s credentials and previous work before proceeding with the surgery.
Open communication with the surgical team is also vital in addressing any concerns or questions, ensuring that patients are well-informed about the procedure and its potential outcomes. Understanding the risks and having realistic expectations can significantly contribute to a positive surgical experience.
- Infection and bleeding risks
- Possibility of asymmetry
- Importance of choosing a qualified surgeon
- Open communication with the surgical team

Leave a Reply